Celiac Disease: Symptoms, Causes, Diagnosis and Treatment

Celiac disease is a chronic autoimmune disorder that affects the small intestine. It is estimated to affect approximately 1% of the global population, making it one of the most common autoimmune diseases worldwide. Despite its prevalence, celiac disease often goes undiagnosed or misdiagnosed, leading to long-term health complications. Therefore, it is crucial to have a comprehensive understanding of this disease in order to promote early diagnosis and effective management.
Table of Contents
Key Takeaways
- Celiac Disease is an autoimmune disorder that damages the small intestine when gluten is consumed.
- Common symptoms of Celiac Disease include abdominal pain, bloating, diarrhea, and weight loss.
- Diagnosis of Celiac Disease involves blood tests, endoscopy, and biopsy of the small intestine.
- Genetics play a role in Celiac Disease, with certain genes increasing the risk of developing the condition.
- Gluten sensitivity and Celiac Disease are different conditions, with the latter being a more severe and long-term autoimmune disorder.
What is Celiac Disease and How Does it Affect the Body?
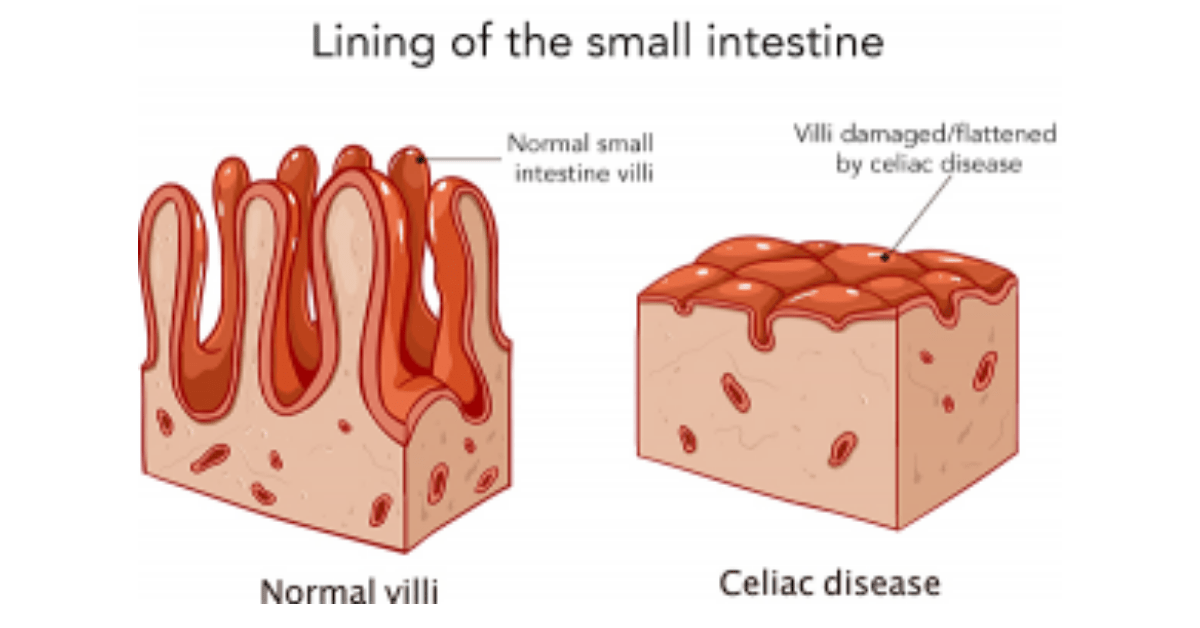
Celiac disease is an autoimmune disorder in which the body’s immune system mistakenly attacks the small intestine when gluten, a protein found in wheat, barley, and rye, is ingested. This immune response damages the lining of the small intestine, leading to inflammation and interfering with the absorption of nutrients from food. Over time, this can result in malnutrition and various health complications.
The immune response triggered by gluten in individuals with celiac disease can cause a wide range of symptoms and affect multiple systems in the body. Digestive symptoms such as abdominal pain, bloating, diarrhea, and constipation are common. However, celiac disease can also manifest with non-digestive symptoms such as fatigue, anemia, bone and joint pain, skin rashes, and even neurological symptoms like headaches and depression.
Common Symptoms of Celiac Disease: Understanding the Signs
The symptoms of celiac disease can vary greatly from person to person, making it challenging to diagnose. Some individuals may experience severe digestive symptoms, while others may have no digestive symptoms at all. Additionally, the severity and frequency of symptoms can fluctuate over time.
Digestive symptoms of celiac disease may include abdominal pain, bloating, gas, diarrhea, constipation, and weight loss. Non-digestive symptoms can include fatigue, anemia (low red blood cell count), osteoporosis (weak bones), dermatitis herpetiformis (a skin rash), and neurological symptoms such as headaches and depression.
It is important to note that not all individuals with celiac disease will experience the same symptoms, and some may have no symptoms at all. This variability in symptoms can make it difficult to recognize and diagnose the disease.
How is Celiac Disease Diagnosed? Tests and Procedures Explained
Diagnosing celiac disease involves a combination of blood tests, biopsy, genetic testing, and other diagnostic tools. The first step in the diagnostic process is usually a blood test to check for specific antibodies that are present in individuals with celiac disease. If the blood test results are positive, a biopsy of the small intestine is typically performed to confirm the diagnosis.
During a biopsy, a small sample of tissue is taken from the lining of the small intestine and examined under a microscope for signs of damage. Genetic testing can also be done to determine if an individual has the specific genes associated with celiac disease.
In some cases, additional diagnostic tools such as imaging studies or capsule endoscopy may be used to further evaluate the extent of intestinal damage or rule out other conditions that may be causing similar symptoms.
The Role of Genetics in Celiac Disease: Causes and Risk Factors
Celiac disease has a strong genetic component, meaning that individuals with certain genes are more likely to develop the disease. The HLA-DQ2 and HLA-DQ8 genes are the most commonly associated genes with celiac disease. However, having these genes does not guarantee that an individual will develop the disease, as there are other factors involved.
Environmental factors also play a role in the development of celiac disease. The most significant environmental factor is exposure to gluten. It is believed that individuals with a genetic predisposition to celiac disease develop an immune response to gluten that triggers the autoimmune reaction in the small intestine.
Other risk factors for developing celiac disease include having a family history of the disease, having other autoimmune disorders such as type 1 diabetes or autoimmune thyroid disease, and being of European descent.
Gluten Sensitivity vs. Celiac Disease: What’s the Difference?

Gluten sensitivity, also known as non-celiac gluten sensitivity, is a condition in which individuals experience symptoms similar to those of celiac disease when they consume gluten. However, unlike celiac disease, gluten sensitivity does not cause damage to the small intestine.
The main difference between gluten sensitivity and celiac disease is the immune response that occurs in the body. In celiac disease, the immune system mounts an autoimmune response against gluten, leading to inflammation and damage to the small intestine. In gluten sensitivity, the immune response is not autoimmune in nature and does not cause intestinal damage.
Despite these differences, there are some similarities between gluten sensitivity and celiac disease. Both conditions can cause similar symptoms such as abdominal pain, bloating, and diarrhea. Additionally, both conditions require a gluten-free diet to manage symptoms.
Gluten-Free Diet: The Key to Managing Celiac Disease
The primary treatment for celiac disease is a strict gluten-free diet. This means avoiding all foods and products that contain gluten, including wheat, barley, rye, and any derivatives of these grains. Following a gluten-free diet can be challenging as gluten is found in many common foods and ingredients.
Foods to avoid on a gluten-free diet include bread, pasta, cereals, baked goods, beer, and many processed foods that may contain hidden sources of gluten. However, there are also many naturally gluten-free foods that can be enjoyed, such as fruits, vegetables, meats, fish, dairy products, and grains like rice and quinoa.
It is important for individuals with celiac disease to carefully read food labels and be aware of cross-contamination risks when preparing or eating food. Cross-contamination can occur when gluten-free foods come into contact with gluten-containing foods or surfaces, leading to unintentional ingestion of gluten.
Medications and Supplements for Celiac Disease: Treatment Options
In addition to following a gluten-free diet, there are medications and supplements that can help manage the symptoms and complications of celiac disease. Medications such as antacids, anti-diarrheal drugs, and corticosteroids may be prescribed to relieve digestive symptoms.
Supplements may also be recommended to address nutrient deficiencies that can occur as a result of malabsorption in the small intestine. Common nutrient deficiencies in individuals with celiac disease include iron, calcium, vitamin D, vitamin B12, and folate. These deficiencies can be managed with appropriate supplementation under the guidance of a healthcare professional.
Probiotics, which are beneficial bacteria that promote gut health, may also be beneficial for individuals with celiac disease. Probiotics can help restore the balance of gut bacteria and improve digestion and nutrient absorption.
Coping with Celiac Disease: Lifestyle Changes and Support Groups
Managing celiac disease requires significant lifestyle changes to ensure strict adherence to a gluten-free diet. This can be challenging, as gluten is present in many common foods and ingredients. It may require careful meal planning, reading food labels, and avoiding cross-contamination in the kitchen.
Support groups can play a crucial role in helping individuals cope with the challenges of living with celiac disease. Support groups provide a sense of community, information sharing, and emotional support for individuals and their families. They can also provide practical tips and resources for managing a gluten-free lifestyle.
In addition to support groups, counseling or therapy may be beneficial for individuals struggling with the emotional impact of living with a chronic condition like celiac disease. It is important to address any feelings of frustration, isolation, or anxiety that may arise from the challenges of managing the disease.
Complications of Untreated Celiac Disease: Long-term Risks
If left untreated, celiac disease can lead to long-term health complications. The chronic inflammation and damage to the small intestine can result in malnutrition and deficiencies in essential nutrients. This can lead to a wide range of health problems, including osteoporosis, anemia, infertility, neurological disorders, and an increased risk of certain types of cancer.
Early diagnosis and treatment are crucial to prevent these long-term complications. It is important for individuals with symptoms suggestive of celiac disease to seek medical attention and undergo appropriate testing to confirm or rule out the diagnosis.
Celiac Disease in Children: Symptoms, Diagnosis, and Treatment
Celiac disease can occur at any age, including childhood. In children, the symptoms of celiac disease may be different from those seen in adults. Common symptoms in children include diarrhea, poor growth or weight loss, abdominal pain, irritability, and delayed puberty.
Diagnosing celiac disease in children involves similar tests and procedures as in adults. Blood tests to check for specific antibodies are usually the first step, followed by a biopsy of the small intestine to confirm the diagnosis.
Treatment for celiac disease in children is also centered around a strict gluten-free diet. It is important for parents and caregivers to provide appropriate support and education to ensure that children adhere to the diet and receive proper nutrition.
Celiac disease is a chronic autoimmune disorder that affects the small intestine. It is important to have a comprehensive understanding of this disease in order to promote early diagnosis and effective management. Common symptoms of celiac disease can vary greatly from person to person, making it challenging to diagnose. Diagnostic tests such as blood tests, biopsy, genetic testing, and other tools are used to confirm the diagnosis. Treatment for celiac disease involves following a strict gluten-free diet and may also include medications, supplements, and probiotics. Support groups and counseling can help individuals cope with the challenges of living with celiac disease. Early diagnosis and treatment are crucial to prevent long-term complications.
If you’re looking for more information on the health benefits and side effects of certain food products, you might find this article on Suja Mighty Dozen Review interesting. It delves into the benefits and potential side effects of Suja’s Mighty Dozen juice blend, which contains a variety of fruits and vegetables known for their nutritional value. Understanding the impact of different foods on our bodies can be especially important for individuals with conditions like Celiac Disease, as they often need to be mindful of their diet choices. Check out the article here to learn more about how certain food products can affect your health.
FAQs
What is celiac disease?
Celiac disease is an autoimmune disorder that affects the small intestine. It is triggered by the consumption of gluten, a protein found in wheat, barley, and rye.
What are the symptoms of celiac disease?
Symptoms of celiac disease can vary widely and may include abdominal pain, bloating, diarrhea, constipation, fatigue, weight loss, and anemia.
What causes celiac disease?
Celiac disease is caused by an abnormal immune response to gluten. The exact cause of this immune response is not yet fully understood, but it is believed to be a combination of genetic and environmental factors.
How is celiac disease diagnosed?
Celiac disease is typically diagnosed through a combination of blood tests and a biopsy of the small intestine. Blood tests can detect the presence of certain antibodies that are produced in response to gluten, while a biopsy can confirm the presence of damage to the small intestine.
What is the treatment for celiac disease?
The only effective treatment for celiac disease is a strict gluten-free diet. This means avoiding all foods and products that contain wheat, barley, and rye. In some cases, additional supplements or medications may be recommended to help manage symptoms or address nutrient deficiencies.