Understanding Celiac Disease: Definition and Overview
Celiac disease is a chronic autoimmune disorder that affects the small intestine and is triggered by the consumption of gluten. Gluten is a protein found in wheat, barley, and rye. When individuals with celiac disease consume gluten, their immune system responds by attacking the lining of the small intestine, causing inflammation and damage. This damage can lead to a variety of symptoms and long-term complications if left untreated. It is important for individuals who may be at risk for celiac disease to understand the disease and its impact on the body.
Table of Contents
Key Takeaways
- Celiac disease is an autoimmune disorder that damages the small intestine when gluten is consumed.
- Celiac disease affects approximately 1% of the population, with higher rates in certain groups such as those with a family history or other autoimmune disorders.
- Symptoms of celiac disease can vary widely and may include digestive issues, fatigue, and skin rashes. Diagnosis involves blood tests and a biopsy of the small intestine.
- Gluten, a protein found in wheat, barley, and rye, triggers the immune response in celiac disease. A gluten-free diet is the only treatment for celiac disease.
- Proper nutrition is crucial for celiac disease patients, as the condition can lead to malabsorption of nutrients. Untreated celiac disease can lead to serious complications such as osteoporosis and an increased risk of certain cancers.
What is Celiac Disease and How Does it Affect the Body?
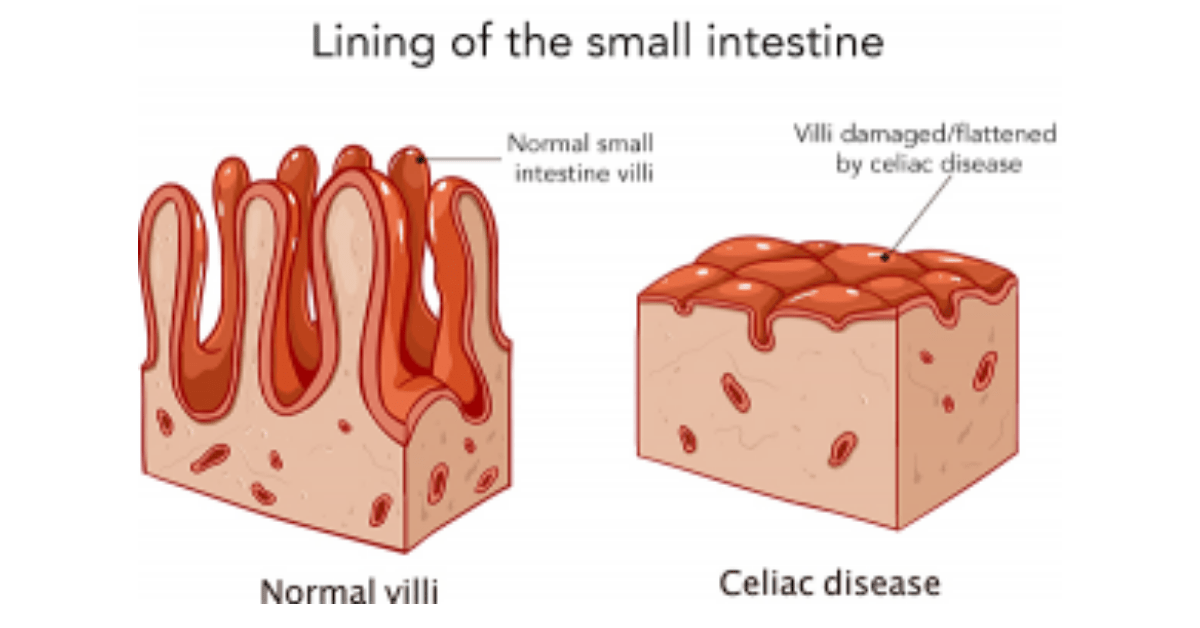
Celiac disease is a genetic autoimmune disorder in which the body’s immune system mistakenly attacks the small intestine when gluten is consumed. The immune response causes inflammation and damage to the lining of the small intestine, specifically the villi, which are finger-like projections that help with nutrient absorption. Over time, this damage can lead to malabsorption of nutrients and a variety of symptoms.
The immune response in celiac disease is triggered by gluten, a protein found in wheat, barley, and rye. When individuals with celiac disease consume gluten, their immune system produces antibodies that attack the lining of the small intestine. This immune response causes inflammation and damage to the villi, leading to a range of symptoms such as abdominal pain, diarrhea, fatigue, and weight loss.
The Prevalence of Celiac Disease: Who is at Risk?
Celiac disease is estimated to affect approximately 1% of the global population. However, it is believed that many cases go undiagnosed or misdiagnosed due to a lack of awareness and understanding of the disease. Celiac disease can occur at any age, from infancy to adulthood.
There are several risk factors associated with celiac disease. One of the primary risk factors is genetics. Individuals who have a first-degree relative with celiac disease, such as a parent or sibling, have a significantly higher risk of developing the disease themselves. Other risk factors include having other autoimmune disorders, such as type 1 diabetes or autoimmune thyroid disease, and having certain genetic markers associated with celiac disease.
Early detection and diagnosis of celiac disease are crucial in order to prevent long-term complications and manage symptoms effectively. It is important for individuals who may be at risk to be aware of the symptoms and seek medical attention if they suspect they may have celiac disease.
Symptoms and Diagnosis of Celiac Disease
The symptoms of celiac disease can vary widely from person to person. Some individuals may experience classic symptoms such as abdominal pain, diarrhea, and weight loss, while others may have more subtle symptoms or no symptoms at all. This variability in symptoms can make diagnosis challenging.
There are several diagnostic tests that can be used to confirm a diagnosis of celiac disease. Blood tests can measure the levels of certain antibodies that are produced in response to gluten consumption. These antibodies, such as anti-tissue transglutaminase (tTG) and anti-endomysial (EMA) antibodies, are often elevated in individuals with celiac disease. If blood tests suggest celiac disease, an endoscopy may be performed to examine the lining of the small intestine and confirm the diagnosis.
However, diagnosing celiac disease can be challenging due to several factors. First, some individuals may not have elevated levels of antibodies in their blood, making it difficult to detect the disease through blood tests alone. Additionally, individuals who follow a gluten-free diet prior to testing may have false-negative results. It is important for individuals who suspect they may have celiac disease to work closely with their healthcare provider to ensure an accurate diagnosis.
The Link Between Celiac Disease and Gluten
Gluten is a protein found in wheat, barley, and rye. In individuals with celiac disease, consuming gluten triggers an immune response that damages the lining of the small intestine. This immune response is specific to gluten and does not occur in individuals without celiac disease.
Following a gluten-free diet is the only treatment for celiac disease. This means avoiding all sources of gluten, including foods made with wheat, barley, and rye. Many individuals with celiac disease find relief from their symptoms by eliminating gluten from their diet.
However, following a gluten-free diet can be challenging. Gluten is found in a wide variety of foods and can also be present in medications, supplements, and personal care products. Cross-contamination is another concern, as even small amounts of gluten can trigger a reaction in individuals with celiac disease. It is important for individuals with celiac disease to carefully read labels and be vigilant about avoiding gluten.
How Gluten-Free Diets Can Help Manage Celiac Disease
A gluten-free diet is the only treatment for celiac disease and can help manage symptoms and prevent long-term complications. When individuals with celiac disease eliminate gluten from their diet, the inflammation and damage to the small intestine can heal, allowing for improved nutrient absorption and overall health.
Following a gluten-free diet can be challenging, but there are many resources available to help individuals with celiac disease navigate their dietary needs. Working with a registered dietitian who specializes in celiac disease can be extremely helpful in developing a meal plan that meets nutritional needs while avoiding gluten. It is also important to read labels carefully and be aware of hidden sources of gluten.
While a gluten-free diet can be effective in managing celiac disease, there are some potential drawbacks and challenges. Gluten-free products are often more expensive than their gluten-containing counterparts and may not be as readily available in all areas. Additionally, some individuals may find it difficult to adhere to a strict gluten-free diet, especially in social situations or when dining out. It is important for individuals with celiac disease to find support and develop strategies for managing these challenges.
The Importance of Proper Nutrition for Celiac Disease Patients
Proper nutrition is crucial for individuals with celiac disease, as the inflammation and damage to the small intestine can lead to nutrient deficiencies. Common nutrient deficiencies in celiac disease include iron, calcium, vitamin D, and B vitamins.
Working with a registered dietitian who specializes in celiac disease can help ensure that individuals with the disease are meeting their nutritional needs. A dietitian can provide guidance on gluten-free alternatives and help individuals develop meal plans that are balanced and nutrient-rich. It is also important for individuals with celiac disease to be aware of fortified gluten-free foods, which can help address nutrient deficiencies.
Potential Complications of Untreated Celiac Disease
If left untreated, celiac disease can lead to a variety of long-term complications. The inflammation and damage to the small intestine can result in malabsorption of nutrients, leading to deficiencies in essential vitamins and minerals. This can cause a range of symptoms such as fatigue, anemia, osteoporosis, and neurological issues.
Untreated celiac disease is also associated with an increased risk of developing other autoimmune disorders, such as type 1 diabetes, autoimmune thyroid disease, and rheumatoid arthritis. Additionally, individuals with untreated celiac disease have a higher risk of developing certain types of cancer, such as lymphoma and small bowel cancer.
Early detection and treatment of celiac disease are crucial in order to prevent these long-term complications. It is important for individuals who suspect they may have celiac disease to seek medical attention and undergo appropriate testing.
Living with Celiac Disease: Coping Strategies and Support
Living with celiac disease can present a variety of challenges, both emotional and social. Individuals with celiac disease may feel isolated or excluded in social situations where food is involved. They may also experience anxiety or stress related to managing their dietary needs and avoiding gluten.
Coping strategies and support are important for individuals with celiac disease. Joining a support group or connecting with others who have celiac disease can provide a sense of community and understanding. Therapy or counseling can also be helpful in managing the emotional challenges of living with a chronic illness.
Self-care and stress management are also important for individuals with celiac disease. Engaging in activities that bring joy and relaxation, such as exercise, hobbies, or spending time with loved ones, can help reduce stress and improve overall well-being.
Celiac Disease and Other Autoimmune Disorders
There is a strong link between celiac disease and other autoimmune disorders. Individuals with celiac disease have an increased risk of developing other autoimmune disorders, and vice versa. The exact relationship between celiac disease and other autoimmune disorders is not fully understood, but it is believed to be related to shared genetic factors and immune system dysfunction.
The symptoms of celiac disease can overlap with those of other autoimmune disorders, making diagnosis challenging. It is important for individuals who have been diagnosed with one autoimmune disorder to be aware of the potential risk for developing others and to seek appropriate medical care.
Comprehensive medical care is crucial for individuals with multiple autoimmune disorders. This may involve working with a team of healthcare providers, including gastroenterologists, endocrinologists, rheumatologists, and dietitians, to manage symptoms and prevent complications.
Research and Advances in Celiac Disease Treatment and Management
There is ongoing research into celiac disease aimed at improving the lives of those affected by the disease. Current research focuses on several areas, including potential new treatments, improved diagnostic tests, and better understanding of the underlying mechanisms of the disease.
One area of research is the development of medications that can help individuals with celiac disease tolerate gluten. These medications work by targeting the immune response to gluten and reducing inflammation in the small intestine. While these medications are still in the experimental stage, they hold promise for the future treatment of celiac disease.
Another area of research is the development of improved diagnostic tests for celiac disease. Current diagnostic tests have limitations, and researchers are working on developing more accurate and reliable tests that can detect celiac disease in individuals who may not have elevated levels of antibodies in their blood.
Ongoing research is crucial for improving the lives of those with celiac disease and advancing our understanding of the disease. It is important for individuals with celiac disease to stay informed about current research and discuss any potential new treatments or management strategies with their healthcare provider.
Celiac disease is a chronic autoimmune disorder that affects the small intestine and is triggered by the consumption of gluten. It is important for individuals who may be at risk for celiac disease to understand the disease and its impact on the body. Early detection and diagnosis are crucial in order to prevent long-term complications and manage symptoms effectively.
Following a gluten-free diet is the only treatment for celiac disease and can help manage symptoms and prevent long-term complications. Proper nutrition is also important for individuals with celiac disease, as the inflammation and damage to the small intestine can lead to nutrient deficiencies.
Living with celiac disease can present challenges, both emotional and social. Coping strategies, support, and self-care are important for individuals with celiac disease. There is ongoing research into celiac disease aimed at improving treatment and management strategies, and it is important for individuals with celiac disease to stay informed about current research.
If you’re interested in learning more about the potential complications of celiac disease, including some lesser-known symptoms and their impact on the skin, check out this informative article: Complications of Celiac Disease: Causes, Interesting Facts, Skin, and Weird Symptoms of Celiac Disease. It provides valuable insights into the risk factors and complications associated with this autoimmune disorder.
FAQs
What is celiac disease?
Celiac disease is an autoimmune disorder that affects the small intestine. It is triggered by the consumption of gluten, a protein found in wheat, barley, and rye.
What are the symptoms of celiac disease?
Symptoms of celiac disease can vary widely and may include abdominal pain, bloating, diarrhea, constipation, fatigue, and weight loss. Some people with celiac disease may also experience skin rashes, joint pain, and anemia.
How is celiac disease diagnosed?
Celiac disease is typically diagnosed through a combination of blood tests and a biopsy of the small intestine. Blood tests can detect the presence of certain antibodies that are produced in response to gluten, while a biopsy can confirm the presence of damage to the small intestine.
What is the treatment for celiac disease?
The only treatment for celiac disease is a strict gluten-free diet. This means avoiding all foods and products that contain wheat, barley, and rye. In some cases, people with celiac disease may also need to avoid oats.
What are the long-term effects of celiac disease?
If left untreated, celiac disease can lead to a range of long-term health problems, including malnutrition, osteoporosis, and an increased risk of certain types of cancer. However, with a strict gluten-free diet, most people with celiac disease can avoid these complications and lead healthy, normal lives.