Genetic Testing for Celiac Disease: Benefits and Drawbacks

Celiac disease is an autoimmune disorder that affects the small intestine and is triggered by the consumption of gluten, a protein found in wheat, barley, and rye. It is estimated that approximately 1% of the global population has celiac disease, but many cases go undiagnosed. The diagnosis of celiac disease can be challenging due to its wide range of symptoms and the limitations of traditional diagnostic methods. However, genetic testing has emerged as a valuable tool in the diagnosis of celiac disease, providing early detection and improved accuracy.
Table of Contents
Key Takeaways
- Celiac disease is an autoimmune disorder triggered by gluten consumption that damages the small intestine.
- Diagnosis of celiac disease involves blood tests, endoscopy, and biopsy of the small intestine.
- Genetic testing can identify the presence of specific genes associated with celiac disease, but it cannot diagnose the disease itself.
- Benefits of genetic testing for celiac disease include identifying at-risk family members and avoiding unnecessary gluten-free diets.
- Drawbacks of genetic testing for celiac disease include false positives and negatives, as well as potential psychological distress.
What is Celiac Disease and How is it Diagnosed?
Celiac disease is a chronic condition in which the immune system reacts to gluten, causing damage to the lining of the small intestine. This damage can lead to various symptoms, including abdominal pain, diarrhea, weight loss, fatigue, and nutrient deficiencies. In some cases, celiac disease may present with non-gastrointestinal symptoms such as anemia, osteoporosis, infertility, or neurological disorders.
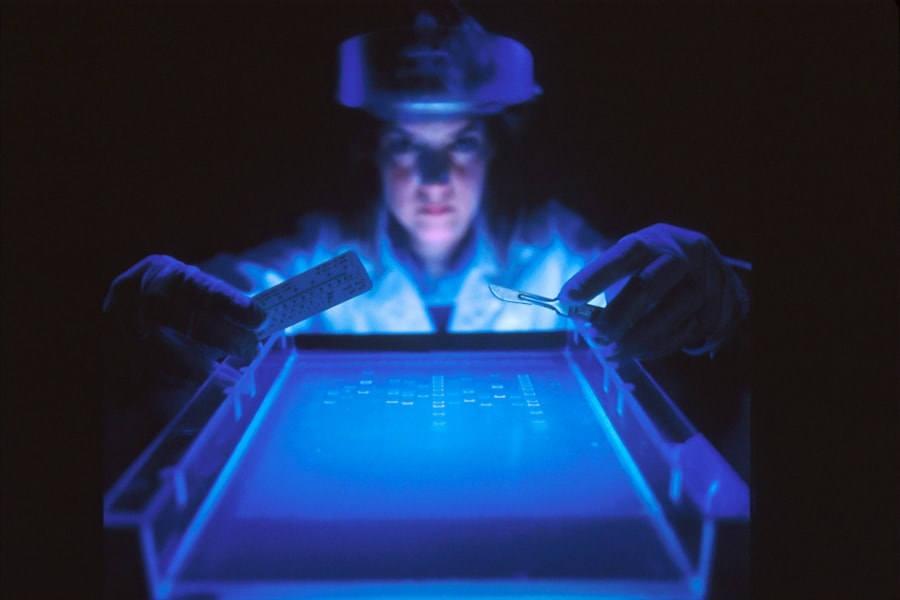
The diagnosis of celiac disease typically involves a combination of clinical evaluation, blood tests, and intestinal biopsies. Blood tests measure the levels of certain antibodies that are elevated in individuals with celiac disease. If these tests indicate the presence of celiac disease, an intestinal biopsy is performed to confirm the diagnosis by examining the damage to the small intestine.
However, these traditional diagnostic methods have limitations. Blood tests can produce false negatives if an individual has already started a gluten-free diet or if they have low levels of the antibodies being measured. Intestinal biopsies can also be inconclusive if there is patchy damage or if the procedure is not performed correctly.
The Role of Genetic Testing in Celiac Disease Diagnosis
Genetic testing for celiac disease involves analyzing an individual’s DNA to identify specific genetic markers associated with the condition. The most common genetic markers associated with celiac disease are the human leukocyte antigen (HLA) genes, specifically HLA-DQ2 and HLA-DQ8. These genes are present in the majority of individuals with celiac disease, although their presence does not guarantee the development of the condition.
Genetic testing can aid in the diagnosis of celiac disease by identifying individuals who are at a higher risk of developing the condition. If an individual tests positive for the HLA-DQ2 or HLA-DQ8 genes, it indicates that they have a genetic predisposition to celiac disease. However, a positive genetic test alone is not sufficient for a diagnosis, as many individuals with these genetic markers do not develop celiac disease.
Benefits of Genetic Testing for Celiac Disease
Genetic testing for celiac disease offers several benefits in the diagnosis and management of the condition. One of the key benefits is early detection and diagnosis. By identifying individuals who are at a higher risk of developing celiac disease, genetic testing allows for earlier intervention and treatment. This can help prevent or minimize the long-term complications associated with untreated celiac disease.
Another benefit of genetic testing is the identification of at-risk family members. Celiac disease has a strong genetic component, and close relatives of individuals with celiac disease have a higher risk of developing the condition themselves. Genetic testing can help identify family members who may benefit from further evaluation and monitoring for celiac disease.
Furthermore, genetic testing improves the accuracy and reliability of celiac disease diagnosis. Traditional diagnostic methods such as blood tests and intestinal biopsies can produce false negatives or inconclusive results. Genetic testing provides additional information that can support or confirm a diagnosis, especially in cases where other diagnostic methods have been inconclusive.
Drawbacks of Genetic Testing for Celiac Disease
While genetic testing for celiac disease offers many benefits, there are also some drawbacks to consider. One potential drawback is the emotional impact of receiving genetic testing results. A positive result may cause anxiety and worry, even if the individual does not currently have celiac disease or may never develop it. On the other hand, a negative result may provide false reassurance, as it does not completely rule out the possibility of developing celiac disease.
Another drawback of genetic testing is the potential for false positives and false negatives. While the presence of certain genetic markers is strongly associated with celiac disease, it is not a definitive diagnosis. Some individuals with celiac disease may not have these genetic markers, while others without celiac disease may test positive for them. Therefore, genetic testing should be used in conjunction with other diagnostic methods to ensure an accurate diagnosis.
Additionally, the availability and accessibility of genetic testing for celiac disease can be limited. Genetic testing may not be covered by insurance or may be prohibitively expensive for some individuals. Furthermore, access to genetic testing may vary depending on geographical location and healthcare system. This can create disparities in access to diagnosis and treatment for individuals with celiac disease.
Genetic Testing for Celiac Disease: Accuracy and Reliability
Genetic testing for celiac disease is highly accurate and reliable when used in conjunction with other diagnostic methods. The presence of the HLA-DQ2 or HLA-DQ8 genes is strongly associated with celiac disease, but it does not guarantee the development of the condition. Therefore, a positive genetic test alone is not sufficient for a diagnosis.
Comparing genetic testing to other diagnostic methods, such as blood tests and intestinal biopsies, each method has its strengths and limitations. Blood tests measure the levels of certain antibodies that are elevated in individuals with celiac disease. However, these tests can produce false negatives if an individual has already started a gluten-free diet or if they have low levels of the antibodies being measured.
Intestinal biopsies are considered the gold standard for diagnosing celiac disease as they directly examine the damage to the small intestine. However, biopsies can be inconclusive if there is patchy damage or if the procedure is not performed correctly. Genetic testing can provide additional information that supports or confirms a diagnosis, especially in cases where other diagnostic methods have been inconclusive.
It is important to note that genetic testing results should be interpreted in the context of an individual’s clinical presentation and other diagnostic findings. Genetic counseling is crucial in helping individuals understand their genetic testing results and make informed decisions about their health.
Genetic Testing vs. Other Celiac Disease Tests: Which is Better?
When it comes to choosing between genetic testing, blood tests, and intestinal biopsies for celiac disease diagnosis, there is no one-size-fits-all answer. Each diagnostic method has its pros and cons, and the best approach may vary depending on individual circumstances.
Genetic testing can provide valuable information about an individual’s risk of developing celiac disease and can help identify at-risk family members. However, it does not provide a definitive diagnosis on its own. Blood tests measure the levels of certain antibodies that are elevated in individuals with celiac disease and can be useful in screening for the condition. However, they can produce false negatives if an individual has already started a gluten-free diet or if they have low levels of the antibodies being measured.
Intestinal biopsies are considered the gold standard for diagnosing celiac disease as they directly examine the damage to the small intestine. However, they are invasive and require a skilled healthcare professional to perform the procedure correctly. Additionally, biopsies can be inconclusive if there is patchy damage or if the procedure is not performed correctly.
The best approach to celiac disease diagnosis is often a combination of these diagnostic methods, taking into account an individual’s clinical presentation, genetic testing results, and other diagnostic findings. This allows for a more comprehensive evaluation and increases the accuracy and reliability of the diagnosis.
Genetic Testing for Celiac Disease: Cost and Accessibility
The cost and accessibility of genetic testing for celiac disease can vary depending on several factors. In some cases, genetic testing may be covered by insurance, especially if there is a family history of celiac disease or if an individual has symptoms suggestive of the condition. However, coverage policies can vary, and some insurance plans may not cover genetic testing for celiac disease.
For individuals without insurance coverage, the out-of-pocket cost of genetic testing can be significant. The cost of genetic testing can range from a few hundred to a few thousand dollars, depending on the specific test and the laboratory performing the analysis. This cost can be a barrier to access for many individuals, especially those with limited financial resources.
Furthermore, the availability of genetic testing for celiac disease can vary depending on geographical location and healthcare system. In some regions, genetic testing may only be available at specialized laboratories or academic medical centers. This can create disparities in access to diagnosis and treatment for individuals with celiac disease, particularly in rural or underserved areas.
Efforts are being made to improve the accessibility of genetic testing for celiac disease, including advocating for insurance coverage and increasing the availability of testing in different regions. However, there is still work to be done to ensure that all individuals who could benefit from genetic testing have access to this valuable diagnostic tool.
Ethical Considerations of Genetic Testing for Celiac Disease
Genetic testing for celiac disease raises several ethical concerns that need to be addressed. One of the main concerns is informed consent and privacy. Individuals undergoing genetic testing should be fully informed about the purpose, benefits, limitations, and potential implications of the test. They should have the opportunity to ask questions and make an informed decision about whether or not to proceed with testing.
Privacy is another important consideration in genetic testing. Genetic information is highly personal and sensitive, and individuals should have control over who has access to their genetic testing results. There is a risk of potential discrimination and stigmatization based on genetic testing results, and individuals should be protected from such harm.
Genetic counseling plays a crucial role in addressing these ethical concerns. Genetic counselors are trained professionals who can provide information, support, and guidance to individuals undergoing genetic testing. They can help individuals understand their genetic testing results, navigate the potential implications, and make informed decisions about their health.
Genetic Testing for Celiac Disease: Implications for Family Members
Genetic testing for celiac disease not only has implications for the individual being tested but also for their family members. Celiac disease has a strong genetic component, and close relatives of individuals with celiac disease have a higher risk of developing the condition themselves. Genetic testing can help identify family members who may benefit from further evaluation and monitoring for celiac disease.
The identification of at-risk family members through genetic testing can have both positive and negative implications. On one hand, it allows for early detection and intervention, which can help prevent or minimize the long-term complications associated with untreated celiac disease. On the other hand, it may cause anxiety and worry for family members who test positive for the genetic markers associated with celiac disease.
Communication and support within families are crucial in navigating the implications of genetic testing results. Open and honest communication can help family members understand the potential risks and benefits of further evaluation and monitoring for celiac disease. Support from healthcare professionals, such as genetic counselors, can also provide guidance and reassurance during this process.
Genetic counseling is particularly important in family planning and decision-making. Individuals who test positive for the genetic markers associated with celiac disease may need to consider their reproductive options and discuss the potential risks with their partners. Genetic counselors can provide information about the likelihood of passing on the genetic predisposition to celiac disease and help individuals make informed decisions about family planning.
Making an Informed Decision: Understanding the Pros and Cons of Genetic Testing for Celiac Disease
When considering genetic testing for celiac disease, it is important to understand the pros and cons and make an informed decision based on personal values and circumstances. The benefits of genetic testing include early detection and diagnosis, identification of at-risk family members, and improved accuracy and reliability of diagnosis. However, there are also drawbacks to consider, such as the emotional impact of receiving genetic testing results, the potential for false positives and false negatives, and the limited availability and accessibility of genetic testing.
Individuals should weigh these pros and cons in the context of their own situation and preferences. Some individuals may prioritize early detection and intervention, while others may be more concerned about the potential emotional impact of receiving genetic testing results. It is important to have open and honest discussions with healthcare professionals, such as genetic counselors, who can provide information, support, and guidance in making an informed decision.
There are resources available for further information and support regarding genetic testing for celiac disease. Organizations such as the Celiac Disease Foundation and the National Celiac Association provide educational materials, support groups, and online forums where individuals can connect with others who have undergone genetic testing or are considering it. Genetic counselors can also provide valuable information and support throughout the decision-making process.
Genetic testing has emerged as a valuable tool in the diagnosis of celiac disease, providing early detection and improved accuracy. While genetic testing offers many benefits, there are also drawbacks to consider, such as the emotional impact of receiving genetic testing results, the potential for false positives and false negatives, and the limited availability and accessibility of genetic testing.
Individuals considering genetic testing for celiac disease should weigh these pros and cons in the context of their own situation and preferences. It is important to have open and honest discussions with healthcare professionals, such as genetic counselors, who can provide information, support, and guidance in making an informed decision.
Advocacy for improved access to genetic testing for celiac disease is crucial to ensure that all individuals who could benefit from this valuable diagnostic tool have access to it. By raising awareness and advocating for insurance coverage and increased availability of testing, we can help improve the diagnosis and management of celiac disease and ultimately improve the quality of life for individuals with the condition.
If you’re interested in genetic testing for celiac disease, you may also want to check out this informative article on TurnToBeHealthy.com. Titled “5 Special Tips for Heart and Kidney Failure Symptoms,” it provides valuable insights into recognizing and managing symptoms of heart and kidney failure. Understanding these symptoms can be crucial for individuals with celiac disease, as they may be at a higher risk for developing these conditions. To learn more, click here.
FAQs
What is celiac disease?
Celiac disease is an autoimmune disorder that affects the small intestine. It is triggered by the consumption of gluten, a protein found in wheat, barley, and rye.
What is genetic testing for celiac disease?
Genetic testing for celiac disease involves analyzing a person’s DNA to determine if they carry certain genes that are associated with an increased risk of developing the condition.
What are the benefits of genetic testing for celiac disease?
Genetic testing for celiac disease can help identify individuals who are at an increased risk of developing the condition. This can lead to earlier diagnosis and treatment, which can improve outcomes and prevent complications.
What are the drawbacks of genetic testing for celiac disease?
Genetic testing for celiac disease cannot definitively diagnose the condition, as not all individuals who carry the associated genes will develop the disease. Additionally, a negative genetic test does not necessarily mean that an individual is not at risk for celiac disease.
Who should consider genetic testing for celiac disease?
Individuals with a family history of celiac disease or other autoimmune disorders may consider genetic testing for celiac disease. Additionally, individuals who have symptoms of celiac disease but have not yet been diagnosed may also benefit from genetic testing.
How is celiac disease diagnosed?
Celiac disease is typically diagnosed through a combination of blood tests and a biopsy of the small intestine. Blood tests can detect the presence of certain antibodies that are associated with celiac disease, while a biopsy can confirm the diagnosis by showing damage to the small intestine.