Understanding Celiac Disease Causes and Risk Factors

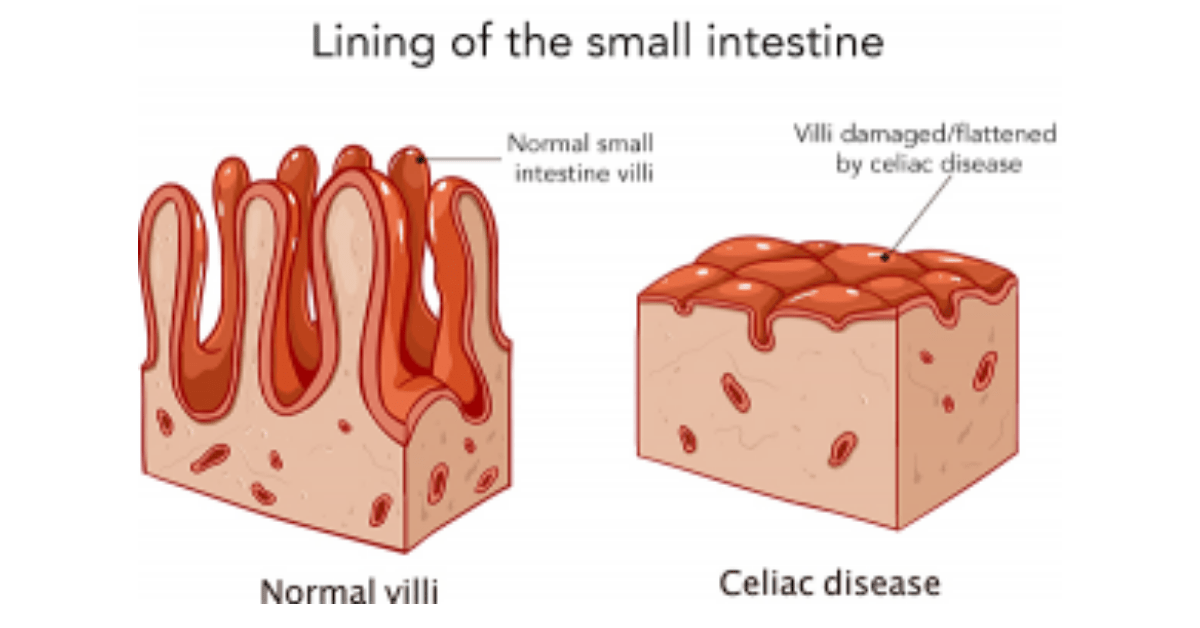
Celiac Disease is an autoimmune disorder that affects the small intestine. It is triggered by the consumption of gluten, a protein found in wheat, barley, and rye. When individuals with Celiac Disease consume gluten, their immune system responds by attacking the lining of the small intestine, leading to inflammation and damage. This damage can interfere with the absorption of nutrients from food, leading to a wide range of symptoms and complications.
The symptoms of Celiac Disease can vary greatly from person to person. Some individuals may experience digestive symptoms such as diarrhea, abdominal pain, and bloating. Others may have non-digestive symptoms such as fatigue, joint pain, and skin rashes. In some cases, Celiac Disease may be asymptomatic, meaning that individuals do not experience any noticeable symptoms.
Diagnosing Celiac Disease can be challenging because the symptoms can be similar to those of other digestive disorders. The gold standard for diagnosis is a biopsy of the small intestine, which involves taking a small sample of tissue to look for signs of damage. Blood tests can also be used to detect certain antibodies that are associated with Celiac Disease. It is important for individuals who suspect they may have Celiac Disease to consult with a healthcare professional for proper diagnosis and management.
Table of Contents
Key Takeaways
- Celiac disease is an autoimmune disorder triggered by gluten consumption.
- Genetics play a significant role in the development of celiac disease.
- Environmental factors such as infections and stress can also trigger celiac disease.
- Gluten sensitivity can lead to similar symptoms as celiac disease but is not an autoimmune disorder.
- Celiac disease can lead to nutritional deficiencies and affect people of all ages, genders, and geographic locations.
Genetics and Celiac Disease
Genetic factors play a significant role in the development of Celiac Disease. It is estimated that about 90% of individuals with Celiac Disease have specific genetic markers known as HLA-DQ2 and HLA-DQ8. These genes are involved in the immune response and are found on certain white blood cells. Having these genes does not guarantee that an individual will develop Celiac Disease, but it does increase the risk.
Family members of individuals with Celiac Disease also have an increased risk of developing the condition. Studies have shown that first-degree relatives (parents, siblings, children) of individuals with Celiac Disease have a 10-20% chance of developing the condition themselves. This suggests that there is a strong genetic component to Celiac Disease. However, it is important to note that not all individuals with the genetic markers will develop the disease, and not all individuals without the markers will be free from the disease.
Environmental Factors and Celiac Disease
While genetics play a significant role in the development of Celiac Disease, environmental factors also play a crucial role. The most well-known environmental trigger for Celiac Disease is gluten consumption. Gluten is found in many common foods, including bread, pasta, and baked goods. When individuals with Celiac Disease consume gluten, it triggers an immune response that leads to inflammation and damage in the small intestine.
However, gluten consumption alone is not enough to cause Celiac Disease. There are likely other environmental triggers that contribute to the development of the condition. For example, studies have shown that certain viral infections may increase the risk of developing Celiac Disease. Additionally, factors such as breastfeeding practices, early introduction of gluten-containing foods, and gut microbiota composition may also play a role in the development of the disease.
Gluten Sensitivity and Celiac Disease
Gluten sensitivity is a condition that shares some similarities with Celiac Disease but does not involve the same autoimmune response. Individuals with gluten sensitivity experience symptoms similar to those of Celiac Disease when they consume gluten, but they do not have the same damage to the small intestine.
There is some overlap between gluten sensitivity and Celiac Disease, as some individuals with gluten sensitivity may go on to develop Celiac Disease later in life. It is estimated that about 10-20% of individuals with gluten sensitivity will eventually develop Celiac Disease. This suggests that gluten sensitivity may be a precursor or early stage of Celiac Disease.
It is important for individuals with gluten sensitivity to work with a healthcare professional to determine if they have Celiac Disease or if they can safely consume gluten without experiencing symptoms. The treatment and management of Celiac Disease and gluten sensitivity may differ, so an accurate diagnosis is crucial.
Autoimmune Disorders and Celiac Disease
Celiac Disease is known to be associated with other autoimmune disorders. Autoimmune disorders occur when the immune system mistakenly attacks healthy cells and tissues in the body. The exact mechanisms behind the association between Celiac Disease and other autoimmune disorders are not fully understood, but it is believed that there may be shared genetic and environmental factors at play.
Some of the autoimmune disorders that are commonly associated with Celiac Disease include type 1 diabetes, autoimmune thyroid disease (such as Hashimoto’s thyroiditis and Graves’ disease), and autoimmune liver diseases (such as autoimmune hepatitis and primary biliary cholangitis). Individuals with Celiac Disease may also have an increased risk of developing other autoimmune disorders such as rheumatoid arthritis, lupus, and Sjögren’s syndrome.
It is recommended that individuals with Celiac Disease undergo screening for other autoimmune disorders, especially if they are experiencing symptoms that are not typical of Celiac Disease. Early detection and management of these conditions can help improve outcomes and quality of life for individuals with Celiac Disease.
Nutritional Deficiencies and Celiac Disease

Celiac Disease can lead to various nutritional deficiencies due to the damage to the small intestine, which impairs the absorption of nutrients from food. Some of the most common nutritional deficiencies seen in individuals with Celiac Disease include iron deficiency anemia, vitamin D deficiency, vitamin B12 deficiency, and calcium deficiency.
The mechanisms behind these nutritional deficiencies in Celiac Disease are multifactorial. The damage to the small intestine can lead to malabsorption of nutrients, especially those that require intact villi for absorption. Additionally, inflammation in the small intestine can impair the production and release of digestive enzymes and hormones that are necessary for proper nutrient absorption.
It is important for individuals with Celiac Disease to work with a healthcare professional to address these nutritional deficiencies. Nutritional supplementation may be necessary to ensure that individuals are getting adequate amounts of essential nutrients. A gluten-free diet alone may not be enough to correct these deficiencies, especially in cases where the damage to the small intestine is severe.
Age and Celiac Disease
Celiac Disease can develop at any age, from infancy to old age. However, the age of onset can vary, and there are some differences in symptoms and diagnosis between children and adults.
In children, Celiac Disease is often diagnosed in early childhood, typically between the ages of 1 and 5. The symptoms in children can vary but may include digestive symptoms such as diarrhea, abdominal pain, and poor growth. Children with Celiac Disease may also experience non-digestive symptoms such as irritability, fatigue, and delayed puberty.
In adults, Celiac Disease can be diagnosed at any age, including later in life. The symptoms in adults can be more varied and may include digestive symptoms as well as non-digestive symptoms such as joint pain, anemia, and infertility. It is not uncommon for adults with Celiac Disease to have no noticeable symptoms or to have symptoms that are mistaken for other conditions.
Older adults with Celiac Disease may be at an increased risk of complications due to the cumulative effects of malabsorption over time. These complications can include osteoporosis, anemia, and neurological disorders. It is important for older adults with Celiac Disease to receive regular monitoring and management to prevent or address these complications.
Gender and Celiac Disease
Celiac Disease can affect individuals of any gender, but there are some differences in prevalence and presentation between men and women. Women are generally more likely to be diagnosed with Celiac Disease than men, with some studies suggesting that the ratio of women to men with Celiac Disease is around 2:1.
Hormonal factors may play a role in the gender differences seen in Celiac Disease. It has been observed that women are more likely to develop Celiac Disease during certain hormonal events such as pregnancy, menopause, and the use of hormonal contraceptives. This suggests that hormones may influence the development and progression of Celiac Disease.
There may also be differences in symptoms and diagnosis between men and women with Celiac Disease. Some studies have suggested that men may be more likely to have atypical or non-digestive symptoms, while women may be more likely to have digestive symptoms. However, more research is needed to fully understand these gender differences.
Geographic Location and Celiac Disease
The prevalence of Celiac Disease varies significantly around the world. It is estimated that the global prevalence of Celiac Disease is around 1%, but this can vary greatly between different countries and regions.
Celiac Disease is most common in Western countries such as Europe, North America, and Australia. In these regions, the prevalence can range from 1-2% or even higher in certain populations. In contrast, Celiac Disease is relatively rare in some Asian countries, with prevalence rates as low as 0.1%.
The reasons for these geographic differences are not fully understood but are likely due to a combination of genetic and environmental factors. For example, certain populations may have a higher prevalence of the HLA-DQ2 and HLA-DQ8 genes, which increase the risk of developing Celiac Disease. Additionally, differences in dietary patterns and exposure to gluten-containing foods may also contribute to the geographic variation in Celiac Disease prevalence.
It is important for healthcare professionals and individuals worldwide to be aware of Celiac Disease and its potential impact on health. Even in areas with low prevalence, individuals may still be at risk for developing the condition, and early diagnosis and management are crucial for preventing complications.
Other Risk Factors for Celiac Disease
In addition to genetic and environmental factors, there are other medical conditions and lifestyle factors that have been associated with an increased risk of developing Celiac Disease.
Some medical conditions that have been linked to an increased risk of Celiac Disease include type 1 diabetes, Down syndrome, Turner syndrome, and autoimmune thyroid disease. Individuals with these conditions should be aware of the potential risk and discuss screening for Celiac Disease with their healthcare provider.
Certain lifestyle factors may also increase the risk of developing Celiac Disease. For example, smoking has been associated with an increased risk of Celiac Disease, while breastfeeding has been shown to have a protective effect. Additionally, individuals who have had repeated gastrointestinal infections or who have undergone certain surgical procedures may be at an increased risk.
It is important for individuals with these risk factors to be aware of the potential for Celiac Disease and to discuss screening and management options with their healthcare provider. Early diagnosis and management can help prevent complications and improve quality of life.
Celiac Disease is a complex autoimmune disorder that is influenced by a combination of genetic and environmental factors. While genetics play a significant role in the development of the disease, environmental triggers such as gluten consumption and viral infections also contribute to its onset. There is also an association between Celiac Disease and other autoimmune disorders, as well as an increased risk of nutritional deficiencies.
The age, gender, and geographic location of individuals can also impact the prevalence, symptoms, and diagnosis of Celiac Disease. It is important for healthcare professionals and individuals to be aware of these factors in order to ensure early diagnosis and appropriate management.
Further research is needed to fully understand the complex nature of Celiac Disease and to develop more effective treatments. In the meantime, it is crucial for individuals with Celiac Disease to work closely with their healthcare providers to manage their condition and prevent complications. With proper diagnosis, management, and awareness, individuals with Celiac Disease can lead healthy and fulfilling lives.
If you’re interested in learning more about the health benefits of natural remedies, you might want to check out this article on Suja Ginger Shot: The Ultimate Immunity Booster for a Healthy Lifestyle. This article explores the powerful effects of ginger and how it can support your immune system. (source)
FAQs
What is celiac disease?
Celiac disease is an autoimmune disorder that affects the small intestine. It is triggered by the consumption of gluten, a protein found in wheat, barley, and rye.
What are the symptoms of celiac disease?
Symptoms of celiac disease can vary widely and may include abdominal pain, bloating, diarrhea, constipation, fatigue, and weight loss.
What are the causes of celiac disease?
The exact cause of celiac disease is unknown, but it is believed to be a combination of genetic and environmental factors. People with a family history of celiac disease are at a higher risk of developing the condition.
What are the risk factors for celiac disease?
Risk factors for celiac disease include having a family history of the condition, having other autoimmune disorders, and being of European descent.
How is celiac disease diagnosed?
Celiac disease is typically diagnosed through blood tests and a biopsy of the small intestine.
What is the treatment for celiac disease?
The only treatment for celiac disease is a strict gluten-free diet. This means avoiding all foods and products that contain wheat, barley, and rye. In some cases, supplements may be recommended to help with nutrient deficiencies.