Non-Classical Celiac Disease: Symptoms and Diagnosis

Non-Classical Celiac Disease, also known as atypical or silent celiac disease, is a form of celiac disease that does not present with the typical gastrointestinal symptoms commonly associated with the condition. Celiac disease is an autoimmune disorder triggered by the ingestion of gluten, a protein found in wheat, barley, and rye. In non-classical celiac disease, individuals may experience a wide range of symptoms that are not directly related to the digestive system.
The prevalence of non-classical celiac disease is not well-established, as it is often underdiagnosed or misdiagnosed due to the absence of typical symptoms. However, studies suggest that it may be more common than classical celiac disease. It is estimated that for every person diagnosed with classical celiac disease, there may be six undiagnosed cases of non-classical celiac disease.
The main difference between classical and non-classical celiac disease lies in the symptoms experienced by individuals. Classical celiac disease is characterized by gastrointestinal symptoms such as diarrhea, abdominal pain, bloating, and weight loss. On the other hand, non-classical celiac disease can present with a wide range of symptoms affecting various systems in the body, including the skin, joints, nervous system, and reproductive system.
Table of Contents
Key Takeaways
- Non-classical celiac disease can present with atypical symptoms and may be difficult to diagnose.
- Symptoms of non-classical celiac disease can include fatigue, joint pain, and neurological issues.
- Early diagnosis of non-classical celiac disease is important to prevent long-term complications.
- Genetic testing can be helpful in diagnosing non-classical celiac disease.
- Non-classical celiac disease is linked to autoimmune disorders and can impact mental health.
Understanding the Symptoms of Non-Classical Celiac Disease
Common symptoms of non-classical celiac disease include fatigue, anemia, osteoporosis, and unexplained weight loss. These symptoms are often attributed to other conditions or dismissed as normal signs of aging. As a result, many individuals with non-classical celiac disease may go undiagnosed for years.
Atypical symptoms of non-classical celiac disease can vary greatly from person to person. Some individuals may experience skin rashes such as dermatitis herpetiformis, which is characterized by itchy blisters and bumps. Others may have joint pain, muscle weakness, or neurological symptoms such as headaches, numbness, or tingling sensations.
The symptoms of non-classical celiac disease can differ from classical celiac disease in several ways. While classical celiac disease primarily affects the digestive system, non-classical celiac disease can affect multiple systems in the body. Additionally, the severity and duration of symptoms may vary among individuals with non-classical celiac disease. Some individuals may have mild and intermittent symptoms, while others may experience chronic and debilitating symptoms.
The Importance of Early Diagnosis
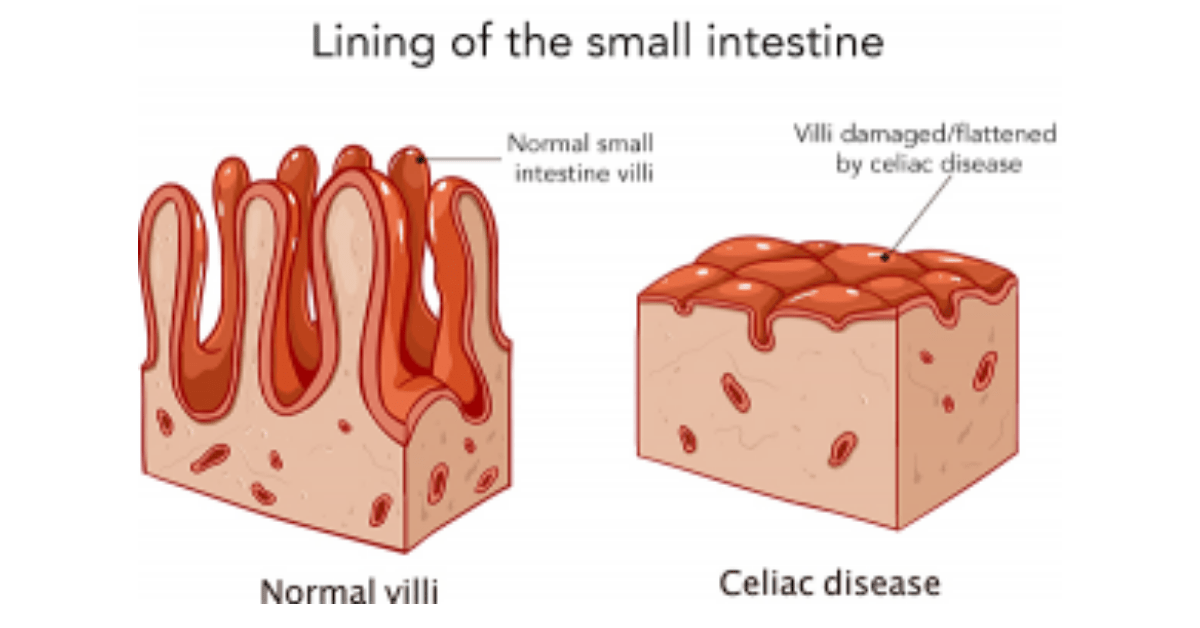
Delayed diagnosis of non-classical celiac disease can have serious consequences for individuals’ health and quality of life. Without proper treatment, the immune system continues to attack the small intestine, leading to inflammation and damage to the intestinal lining. This can result in malabsorption of nutrients, leading to deficiencies in vitamins and minerals.
Long-term consequences of untreated non-classical celiac disease include an increased risk of developing other autoimmune disorders, such as type 1 diabetes, autoimmune thyroid disease, and autoimmune liver disease. There is also an increased risk of developing certain types of cancer, such as lymphoma and small bowel adenocarcinoma.
Early diagnosis of non-classical celiac disease is crucial for preventing these complications and improving overall health outcomes. With a proper diagnosis, individuals can begin a gluten-free diet and receive appropriate medical treatment to manage their symptoms and prevent further damage to the small intestine.
To get diagnosed with non-classical celiac disease, individuals should consult with a healthcare provider who specializes in celiac disease or autoimmune disorders. The diagnostic process typically involves a combination of blood tests to detect specific antibodies associated with celiac disease and an intestinal biopsy to assess the extent of damage to the small intestine.
The Role of Genetic Testing in Non-Classical Celiac Disease
Genetic testing can play a valuable role in the diagnosis of non-classical celiac disease. Celiac disease is strongly associated with specific genetic markers, particularly the human leukocyte antigen (HLA) genes. The presence of certain HLA genes, specifically HLA-DQ2 and HLA-DQ8, increases the risk of developing celiac disease.
Genetic testing involves a simple blood test to determine if an individual carries the HLA-DQ2 or HLA-DQ8 genes. However, it is important to note that genetic testing alone cannot confirm or rule out a diagnosis of celiac disease. While the presence of these genes increases the risk, it does not guarantee that an individual will develop the condition.
Genetic testing can be particularly useful in cases where the diagnosis of non-classical celiac disease is uncertain or when individuals are already following a gluten-free diet. If genetic testing reveals the presence of the HLA-DQ2 or HLA-DQ8 genes, it may indicate a higher likelihood of developing celiac disease in the future and may warrant further evaluation and monitoring.
It is important to note that genetic testing should not be used as a standalone diagnostic tool for celiac disease. A definitive diagnosis requires a combination of genetic testing, blood tests for specific antibodies, and an intestinal biopsy to assess the extent of damage to the small intestine.
The Link between Non-Classical Celiac Disease and Autoimmune Disorders
Non-classical celiac disease is often associated with other autoimmune disorders. Autoimmune disorders occur when the immune system mistakenly attacks healthy cells and tissues in the body. In individuals with non-classical celiac disease, the immune system’s response to gluten can trigger an autoimmune response that affects various systems in the body.
Some common autoimmune disorders associated with non-classical celiac disease include type 1 diabetes, autoimmune thyroid disease (such as Hashimoto’s thyroiditis and Graves’ disease), autoimmune liver diseases (such as primary biliary cholangitis and autoimmune hepatitis), and rheumatoid arthritis.
The exact mechanisms by which non-classical celiac disease triggers autoimmune disorders are not fully understood. However, it is believed that the immune response to gluten in individuals with non-classical celiac disease can lead to systemic inflammation and immune dysregulation, increasing the risk of developing other autoimmune disorders.
It is important for individuals with non-classical celiac disease to be aware of the potential risk of developing other autoimmune disorders and to undergo regular monitoring for early detection and management of these conditions.
The Impact of Non-Classical Celiac Disease on Mental Health

Non-classical celiac disease can have a significant impact on mental health. Research has shown a strong association between celiac disease and various mental health issues, including depression, anxiety, and cognitive impairment.
The connection between non-classical celiac disease and mental health issues is not fully understood, but it is believed to be related to the systemic inflammation and immune dysregulation caused by the immune response to gluten. Inflammation in the brain can disrupt neurotransmitter function and contribute to mood disorders such as depression and anxiety.
Common mental health issues associated with non-classical celiac disease include:
– Depression: Individuals with non-classical celiac disease may experience persistent feelings of sadness, loss of interest in activities, changes in appetite or weight, sleep disturbances, and difficulty concentrating.
– Anxiety: Non-classical celiac disease can contribute to feelings of excessive worry, restlessness, irritability, and physical symptoms such as rapid heartbeat or shortness of breath.
– Cognitive impairment: Some individuals with non-classical celiac disease may experience difficulties with memory, attention, and problem-solving skills. This can affect daily functioning and quality of life.
Managing mental health issues in individuals with non-classical celiac disease often involves a combination of medication, therapy, and lifestyle changes. It is important for individuals to seek support from healthcare professionals who are knowledgeable about the connection between celiac disease and mental health.
The Challenges of Diagnosing Non-Classical Celiac Disease
Non-classical celiac disease can be challenging to diagnose due to several factors. Firstly, the symptoms of non-classical celiac disease can be vague and nonspecific, making it difficult for healthcare providers to recognize the condition. Many individuals with non-classical celiac disease may present with symptoms that are attributed to other conditions or dismissed as unrelated.
Secondly, non-classical celiac disease often does not present with the typical gastrointestinal symptoms associated with classical celiac disease. This can lead to a delay in diagnosis, as healthcare providers may not consider celiac disease as a possible cause of the individual’s symptoms.
Thirdly, there is a lack of awareness and understanding of non-classical celiac disease among healthcare providers. Many healthcare professionals may not be familiar with the atypical symptoms and presentations of celiac disease, leading to misdiagnosis or underdiagnosis.
To overcome these diagnostic challenges, it is important for individuals to advocate for themselves and seek out healthcare providers who are knowledgeable about celiac disease and autoimmune disorders. Keeping a detailed record of symptoms and any potential triggers can also help healthcare providers make an accurate diagnosis.
Treatment Options for Non-Classical Celiac Disease
The primary treatment for non-classical celiac disease is a strict gluten-free diet. This involves avoiding all sources of gluten, including wheat, barley, rye, and any products derived from these grains. Following a gluten-free diet can help manage symptoms, prevent further damage to the small intestine, and reduce the risk of complications associated with celiac disease.
In addition to a gluten-free diet, individuals with non-classical celiac disease may benefit from medications that help manage specific symptoms or complications. For example, individuals with dermatitis herpetiformis may require topical or oral medications to control the skin rash. Those with osteoporosis may need calcium and vitamin D supplements to improve bone health.
Alternative treatments such as probiotics, digestive enzymes, and herbal supplements have been explored for non-classical celiac disease, but their effectiveness is not well-established. It is important to consult with a healthcare provider before starting any alternative treatments to ensure they are safe and appropriate.
The Role of Diet in Managing Non-Classical Celiac Disease
Following a strict gluten-free diet is essential for managing non-classical celiac disease. Gluten can trigger an immune response in individuals with celiac disease, leading to inflammation and damage to the small intestine. By eliminating gluten from the diet, individuals can prevent further damage and alleviate symptoms.
A gluten-free diet involves avoiding all sources of gluten, including wheat, barley, rye, and any products derived from these grains. This includes foods such as bread, pasta, cereals, and baked goods. It is important to carefully read food labels and look for gluten-free certifications to ensure that products are safe to consume.
In addition to food, individuals with non-classical celiac disease should also be mindful of potential sources of gluten in medications, supplements, and personal care products. These products may contain hidden sources of gluten that can inadvertently be ingested.
Maintaining a gluten-free diet can be challenging, especially when dining out or traveling. It is important to plan ahead, communicate with restaurant staff about dietary restrictions, and carry gluten-free snacks or meals when necessary. Working with a registered dietitian who specializes in celiac disease can also be helpful in developing a balanced and nutritious gluten-free meal plan.
Living with Non-Classical Celiac Disease: Coping Strategies and Support Resources
Living with non-classical celiac disease can be challenging, both physically and emotionally. Coping strategies can help individuals manage their symptoms and maintain a positive outlook on life.
Some coping strategies for living with non-classical celiac disease include:
– Educating oneself about celiac disease and gluten-free living: Understanding the condition and how to manage it can empower individuals to make informed decisions about their health and well-being.
– Building a support system: Connecting with others who have celiac disease or joining support groups can provide a sense of community and understanding. It can also be helpful to involve family and friends in the journey to ensure a supportive environment.
– Practicing self-care: Taking care of one’s physical and mental well-being is crucial. This may involve engaging in regular exercise, getting enough sleep, managing stress, and seeking professional help for mental health issues.
– Being prepared: Planning ahead and being proactive can help individuals navigate social situations, travel, and dining out while adhering to a gluten-free diet. Carrying gluten-free snacks or meals, communicating dietary needs to others, and researching gluten-free options in advance can make these situations less stressful.
There are also numerous resources available to support individuals with non-classical celiac disease. These include online communities, support groups, educational websites, cookbooks, and apps that provide information on gluten-free living, recipes, and tips for managing the condition.
In conclusion, non-classical celiac disease is a form of celiac disease that does not present with the typical gastrointestinal symptoms. It is important for individuals experiencing atypical symptoms to seek medical attention and consider the possibility of non-classical celiac disease. Early diagnosis is crucial for preventing complications and improving overall health outcomes. Genetic testing can play a role in the diagnosis of non-classical celiac disease, but it should not be used as a standalone diagnostic tool. Treatment involves following a strict gluten-free diet, and individuals may benefit from medications or alternative treatments to manage specific symptoms or complications. Living with non-classical celiac disease can be challenging, but with proper support and self-care, individuals can lead a healthy and fulfilling life.
If you’re interested in learning more about the potential interactions and precautions of combining omeprazole and turmeric, check out this informative article on TurnToBeHealthy.com. It provides recommended doses, discusses possible interactions, and highlights important precautions to consider. Understanding how these two substances may interact can help you make informed decisions about your health. Read more here. Additionally, if you’re looking for ways to boost your immunity and maintain a healthy lifestyle, the Suja Ginger Shot is worth exploring. This article on TurnToBeHealthy.com explains how this ultimate immunity booster can benefit your overall well-being. Discover more here.
FAQs
What is Non-Classical Celiac Disease?
Non-Classical Celiac Disease is a type of celiac disease that does not present with the typical gastrointestinal symptoms. Instead, it may present with symptoms such as anemia, osteoporosis, infertility, or neurological symptoms.
What are the symptoms of Non-Classical Celiac Disease?
The symptoms of Non-Classical Celiac Disease can vary widely, but may include anemia, osteoporosis, infertility, neurological symptoms such as headaches or numbness, or skin rashes.
How is Non-Classical Celiac Disease diagnosed?
Non-Classical Celiac Disease is diagnosed through a combination of blood tests and intestinal biopsies. Blood tests can detect the presence of certain antibodies, while intestinal biopsies can confirm the presence of damage to the small intestine.
What is the treatment for Non-Classical Celiac Disease?
The treatment for Non-Classical Celiac Disease is a strict gluten-free diet. This means avoiding all foods that contain gluten, including wheat, barley, and rye. In some cases, additional supplements or medications may be necessary to address specific symptoms.
Can Non-Classical Celiac Disease be cured?
There is currently no cure for Non-Classical Celiac Disease. However, following a strict gluten-free diet can effectively manage symptoms and prevent further damage to the small intestine.
Is Non-Classical Celiac Disease common?
Non-Classical Celiac Disease is less common than Classical Celiac Disease, which presents with more typical gastrointestinal symptoms. However, it is estimated that up to 50% of people with celiac disease may have Non-Classical Celiac Disease.