Celiac Disease Diagnosis: Tests and Procedures

Celiac disease is a chronic autoimmune disorder that affects the small intestine and is triggered by the consumption of gluten, a protein found in wheat, barley, and rye. It is estimated to affect approximately 1% of the global population, making it one of the most common autoimmune diseases worldwide. Celiac disease can have a significant impact on individuals, leading to a range of symptoms and complications if left untreated. Early diagnosis and treatment are crucial in managing the disease and preventing long-term complications.
Table of Contents
Key Takeaways
- Celiac disease is an autoimmune disorder triggered by gluten consumption.
- Symptoms of celiac disease include digestive issues, fatigue, and skin rashes.
- Blood tests can detect celiac disease antibodies, but endoscopy and biopsy are the gold standard for diagnosis.
- Genetic testing can determine if someone is at risk for celiac disease, but it cannot diagnose the condition.
- Non-invasive tests for celiac disease are not as reliable as endoscopy and biopsy.
Understanding Celiac Disease and its Diagnosis
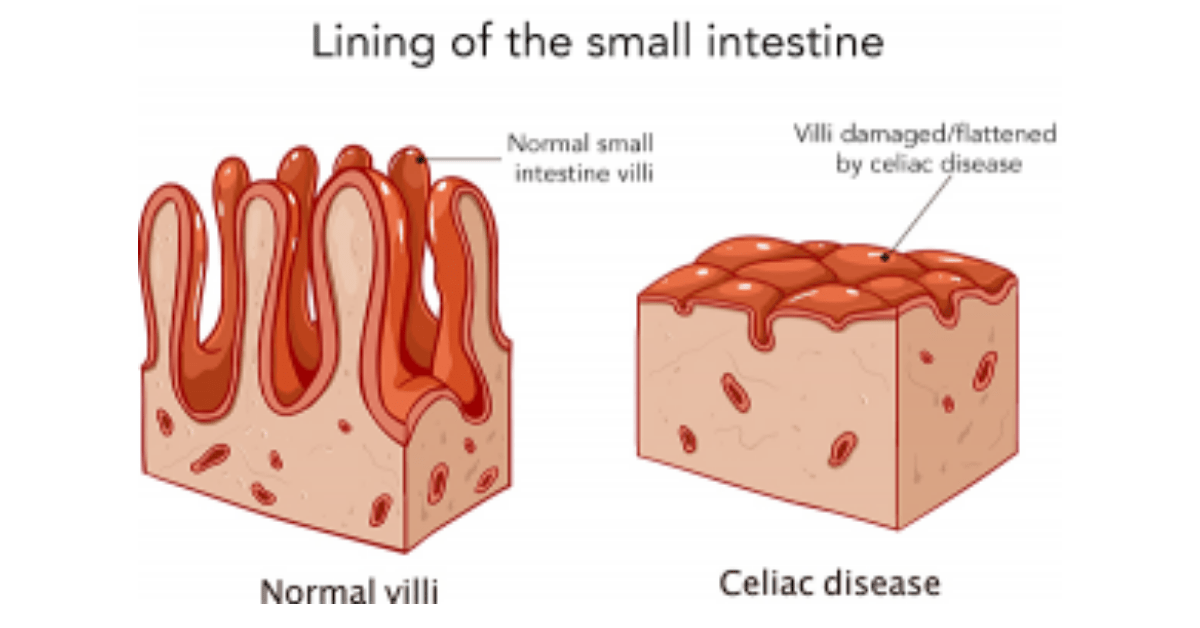
Celiac disease is characterized by an immune response to gluten, which causes inflammation and damage to the lining of the small intestine. This damage can lead to malabsorption of nutrients and a range of symptoms, including abdominal pain, diarrhea, weight loss, fatigue, and skin rashes. The exact cause of celiac disease is unknown, but it is believed to involve a combination of genetic and environmental factors.
The prevalence of celiac disease varies across different populations, with higher rates reported in individuals of European descent. It is estimated that approximately 1 in 100 people worldwide have celiac disease. The incidence rates have been increasing over the past few decades, possibly due to improved awareness and diagnostic methods.
Diagnosing celiac disease can be challenging as the symptoms can vary widely and may overlap with other gastrointestinal disorders. The diagnosis process typically involves a combination of blood tests, endoscopy with biopsy, genetic testing, serology testing, gluten challenge, and ruling out other conditions through differential diagnosis.
Symptoms of Celiac Disease: When to Seek Medical Help
The symptoms of celiac disease can vary from person to person and may range from mild to severe. Common symptoms include abdominal pain, bloating, diarrhea or constipation, weight loss, fatigue, and irritability. However, some individuals may experience atypical symptoms or have no symptoms at all.
Atypical symptoms of celiac disease can include anemia, osteoporosis, infertility, neurological symptoms such as headaches and numbness, and skin rashes such as dermatitis herpetiformis. These atypical symptoms can make the diagnosis process more challenging, as they may not immediately be recognized as being related to celiac disease.
It is important to seek medical help if you suspect you may have celiac disease, especially if you have a family history of the condition or if you are experiencing persistent or severe symptoms. Early diagnosis and treatment can help prevent long-term complications and improve quality of life.
Blood Tests for Celiac Disease: How They Work
Blood tests are often the first step in diagnosing celiac disease. These tests measure the levels of certain antibodies in the blood that are associated with the immune response to gluten. The two main types of blood tests used for celiac disease diagnosis are the tissue transglutaminase (tTG) antibody test and the deamidated gliadin peptide (DGP) antibody test.
The tTG antibody test measures the levels of antibodies that target tissue transglutaminase, an enzyme involved in the immune response to gluten. The DGP antibody test measures the levels of antibodies that target deamidated gliadin peptides, which are fragments of gluten that have been modified by an enzyme.
These blood tests have a high sensitivity and specificity for celiac disease, meaning they are accurate in identifying individuals who have the condition and ruling out those who do not. However, false negatives can occur, especially in individuals who have already started a gluten-free diet or have only mild intestinal damage.
Endoscopy and Biopsy: The Gold Standard for Celiac Diagnosis
Endoscopy with biopsy is considered the gold standard for diagnosing celiac disease. During this procedure, a thin tube with a camera is inserted through the mouth and into the small intestine to visualize the lining of the intestine. Small tissue samples, or biopsies, are taken from the lining of the small intestine and examined under a microscope for signs of damage.
Endoscopy with biopsy is important in celiac diagnosis as it allows for direct visualization of the intestinal lining and assessment of the extent of damage. It can also help rule out other conditions that may have similar symptoms to celiac disease.
However, endoscopy with biopsy is an invasive procedure that requires sedation and carries some risks, such as bleeding and infection. It can also be costly and may not be readily available in all healthcare settings.
Genetic Testing for Celiac Disease: What It Tells You

Genetic testing for celiac disease involves analyzing a person’s DNA to identify specific genetic markers associated with the condition. The most common genetic markers associated with celiac disease are human leukocyte antigen (HLA) genes, specifically HLA-DQ2 and HLA-DQ8.
Genetic testing can be useful in certain situations, such as when there is uncertainty in the diagnosis or when a person has already started a gluten-free diet. If a person does not have the HLA-DQ2 or HLA-DQ8 genes, it is highly unlikely that they have celiac disease.
However, it is important to note that having these genetic markers does not necessarily mean a person will develop celiac disease. Approximately 30-40% of the general population carries these genetic markers, but only a small percentage of them will go on to develop the condition.
Serology Testing: An Alternative to Endoscopy
Serology testing involves measuring the levels of specific antibodies in the blood that are associated with celiac disease. These tests are similar to the blood tests mentioned earlier but may use different markers or techniques.
Serology testing can be an alternative to endoscopy with biopsy in certain situations, such as when a person is unable or unwilling to undergo an invasive procedure. However, it is important to note that serology testing alone is not sufficient for a definitive diagnosis of celiac disease. If the serology tests are positive, further evaluation with endoscopy and biopsy is usually recommended to confirm the diagnosis.
Gluten Challenge: What It Is and How It’s Done
A gluten challenge involves reintroducing gluten into the diet after a period of being on a gluten-free diet. This challenge is done under medical supervision and typically involves consuming a certain amount of gluten daily for a specified period, usually 6-8 weeks.
The purpose of a gluten challenge is to provoke the immune response and induce symptoms in individuals who may have celiac disease. This can help confirm the diagnosis and assess the severity of the condition.
A gluten challenge should only be done under medical supervision, as it can cause significant discomfort and symptoms in individuals with celiac disease. It is important to discuss the risks and benefits of a gluten challenge with a healthcare provider before considering this option.
Non-Invasive Tests for Celiac Disease: Are They Reliable?
Non-invasive tests for celiac disease are being developed as alternatives to traditional diagnostic methods such as endoscopy with biopsy. These tests aim to provide accurate and reliable results without the need for invasive procedures.
One example of a non-invasive test is the use of stool samples to detect specific markers associated with celiac disease. This method has shown promising results in research studies, but further validation is needed before it can be widely used in clinical practice.
Other non-invasive tests being explored include breath tests and urine tests that measure specific markers associated with celiac disease. These tests are still in the early stages of development and require further research before they can be considered reliable diagnostic tools.
Differential Diagnosis: Ruling Out Other Conditions
Differential diagnosis is an important step in the diagnostic process for celiac disease. This involves considering and ruling out other conditions that may have similar symptoms to celiac disease.
Some common conditions that can mimic celiac disease include irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), lactose intolerance, and food allergies. These conditions may require different treatment approaches, so it is important to accurately diagnose celiac disease and rule out other conditions before starting treatment.
Follow-Up Testing: Monitoring Celiac Disease and Treatment Response
Follow-up testing is an important part of managing celiac disease and assessing the response to treatment. This typically involves repeating blood tests to measure antibody levels and monitoring symptoms and dietary adherence.
Follow-up testing can help determine if the gluten-free diet is effectively managing the condition and if any adjustments or additional interventions are needed. It can also help identify any potential complications or associated conditions that may develop over time.
Different types of follow-up testing may be recommended depending on the individual’s specific situation and needs. These may include blood tests, endoscopy with biopsy, or other diagnostic methods as deemed necessary by the healthcare provider.
In conclusion, early diagnosis and treatment of celiac disease are crucial in managing the condition and preventing long-term complications. The diagnosis process for celiac disease can be complex and may involve a combination of blood tests, endoscopy with biopsy, genetic testing, serology testing, gluten challenge, and ruling out other conditions through differential diagnosis.
While blood tests are often the first step in diagnosing celiac disease, endoscopy with biopsy is considered the gold standard for confirmation. Genetic testing and serology testing can provide additional information but are not sufficient for a definitive diagnosis on their own.
Non-invasive tests for celiac disease are being developed as alternatives to traditional diagnostic methods, but further research is needed to validate their accuracy and reliability. Follow-up testing is important in monitoring celiac disease and treatment response, and may involve repeating blood tests, endoscopy with biopsy, or other diagnostic methods as deemed necessary.
Overall, early and accurate diagnosis of celiac disease is essential in managing the condition and improving quality of life for individuals affected by this autoimmune disorder. Continued research and advancements in diagnostic methods will further enhance our understanding and management of celiac disease in the future.
If you’re interested in learning more about the risk factors and complications associated with Celiac Disease, check out this informative article: Celiac Disease Risk Factors and Complications. It provides valuable insights into the various factors that can increase your chances of developing Celiac Disease, as well as the potential complications that can arise if the condition is left untreated. Understanding these aspects can help you take proactive steps towards managing and treating Celiac Disease effectively.
FAQs
What is celiac disease?
Celiac disease is an autoimmune disorder that affects the small intestine. It is triggered by the consumption of gluten, a protein found in wheat, barley, and rye.
What are the symptoms of celiac disease?
Symptoms of celiac disease can vary widely and may include abdominal pain, bloating, diarrhea, constipation, fatigue, and weight loss.
How is celiac disease diagnosed?
Celiac disease is typically diagnosed through a combination of blood tests and a biopsy of the small intestine.
What blood tests are used to diagnose celiac disease?
Blood tests used to diagnose celiac disease include the tTG-IgA test, the EMA-IgA test, and the DGP-IgA test.
What is a small intestine biopsy?
A small intestine biopsy involves taking a small sample of tissue from the lining of the small intestine. This tissue is then examined under a microscope to look for signs of damage or inflammation.
How is a small intestine biopsy performed?
A small intestine biopsy is typically performed during an upper endoscopy procedure. A thin, flexible tube with a camera on the end is inserted through the mouth and into the small intestine. A small tool is then used to take a tissue sample.
Is there a cure for celiac disease?
There is currently no cure for celiac disease. The only treatment is to follow a strict gluten-free diet for life.